As the leading cause of mortality threatening human health, approximately 15 million people worldwide die from cardiovascular and cerebrovascular diseases each year, with over 3 million deaths attributed to acute cardiovascular and cerebrovascular diseases in China alone. According to data from the National Health Commission, in 2021, cardiovascular events accounted for over 40% of total deaths among urban residents in China. Specifically, deaths from heart disease and cerebrovascular disease constituted 25.64% and 21.71% respectively, surpassing the mortality rate from malignant tumors. Traditional treatment methods primarily involve controlling risk factors, medication, and surgical intervention. However, these methods still have certain limitations. It is imperative to explore new therapeutic strategies.

Nanobodies facilitate interactions among inflammatory cells within atherosclerotic plaques and inhibit the further development of inflammatory reactions. Additionally, nanobodies can regulate the immune system and promote plaque stabilization, thereby reducing the risk of cardiovascular events. In stroke therapy, nanobodies leverage their superior penetrative abilities to cross the blood-brain barrier and bind to clots, promoting their dissolution or preventing their binding to the vessel wall, aiding in the treatment of cerebral artery embolism [1]

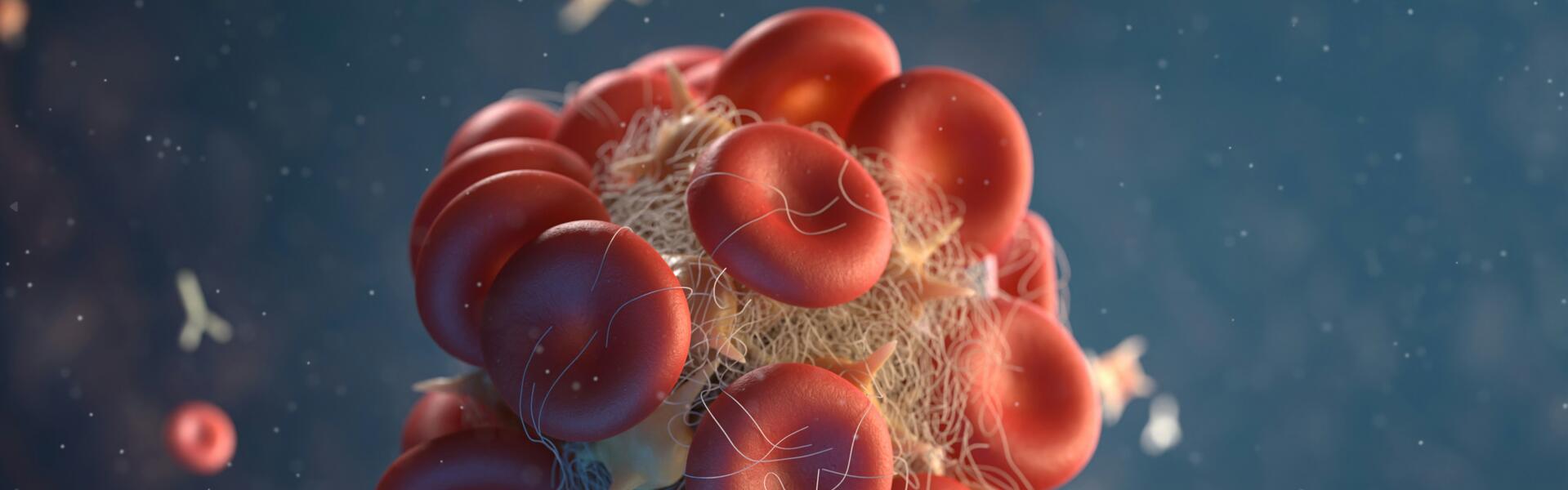
In thrombosis treatment, Caplacizumab, developed by Ablynx and approved by the FDA, selectively inhibits thrombus formation. This humanized anti-von Willebrand factor nanobody demonstrates a favorable therapeutic window in acute thrombosis testing using a baboon safety model [2]. Caplacizumab primarily treats adult-acquired thrombotic thrombocytopenic purpura (TTP). The pathogenesis of acquired TTP involves autoantibodies in patients inhibiting the activity of the von Willebrand factor (vWF)-cleaving protease ADAMTS13, leading to vWF adhesion to platelets and microvascular thrombosis formation. Consequently, tissue ischemia and multi-organ dysfunction may occur, potentially leading to thromboembolic events and death. Caplacizumab binds to the A1 domain of vWF, preventing platelet aggregation and adhesion. Moreover, its binding with vWF prolongs its half-life, which ranges from 10 to 30 hours, similar to reported values for vWF, further validating its mechanism of action [3].
Although nanobodies have achieved remarkable success in diseases like TTP, further exploration in the field of cardiovascular and cerebrovascular diseases is necessary to establish them as a widely applicable and safe therapeutic strategy.